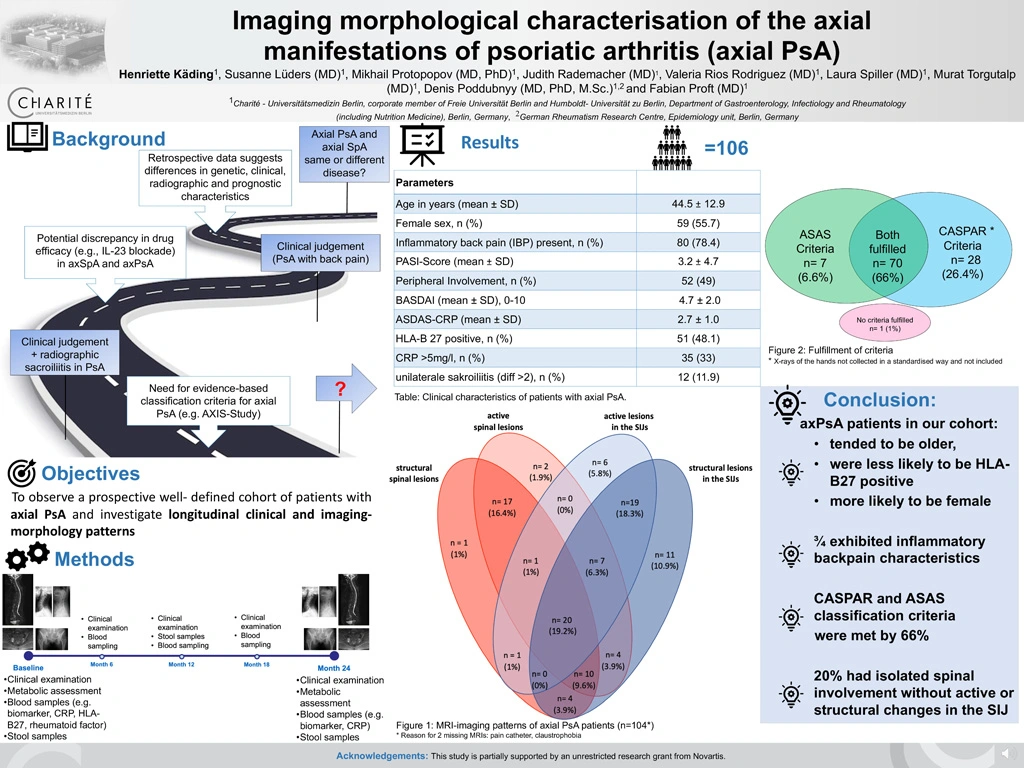
Imaging morphological characterisation of the axial manifestations of psoriatic arthritis (axial PsA)
Authors
Background. Under the umbrella term spondyloarthritis whose clinical presentations are very heterogeneous, psoriatic arthritis (PsA) and axial spondyloarthritis (axSpA) are subsumed together. The presence of axial involvement in patients with PsA (axial PsA) was reported already in 1973 and has been described among others to be present in one third of PsA patients [1]. In the past, retrospective and cross-sectional studies have shown that there are differences in particular: in genetics, clinical presentation, radiographic patterns, as well as in prognostic characteristics [2].
Objective. This study is a prospective, longitudinal, observational study of axial PsA patients to investigate the clinical and imaging morphology patterns of those patients.
Methods. In addition to clinical and laboratory characterization this is the first study to collect in addition to conventional radiographs, MRI of the whole spine and sacroiliac joints (SIJ) according to a standardized protocol from all included patients.
Results. Between August 2019 and June 2023, 106 axial PsA patients were included. The mean age was 44.5 years with a modest majority of females (55.7%). HLA-B27 was positive in half of the patients (48.1%), and C-reactive protein was elevated (>5mg/l) in one third of all patients (33%). Inflammatory back pain (IBP) in the discretion of the treating rheumatologist was commonly present within three quarters of all patients (78.4%). A little less than half of the patients (44.4%) fulfilled the modified New York criteria. In Figure 1 you can see the evaluation of the baseline MRIs divided into active and structural changes in the spine and SIJ. MRI of the SIJ showed active inflammatory changes in half of the patients (51.9%) and structural changes in three quarters (72.1%). While just over half had active inflammation on MRI of the spine (58.7%). Exclusively active and/or structural changes of the spine without changes in the SIJ were seen in 20% of our patients. Figure 2 shows the fulfillment of the ASAS and CASPAR criteria. 92% fulfilled CASPAR criteria for PsA and 73% the ASAS criteria. 66% of patients met both ASAS and CASPAR criteria.
Conclusion. The baseline data of our cohort showed that axial PsA patients are more likely to be female and less likely to be HLA-B27 positive compared to typical axial SpA patients. Both CASPAR and ASAS criteria were met by 66% of patients and an isolated spinal involvement is seen in 20%.
References:
1. Gladman, D.D., et al., Psoriatic arthritis (PSA)--an analysis of 220 patients. Q J Med, 1987. 62(238): p. 127-41.
2. Poddubnyy, D., et al., Axial involvement in psoriatic arthritis: An update for rheumatologists. Semin Arthritis Rheum, 2021. 51(4): p. 880-887.