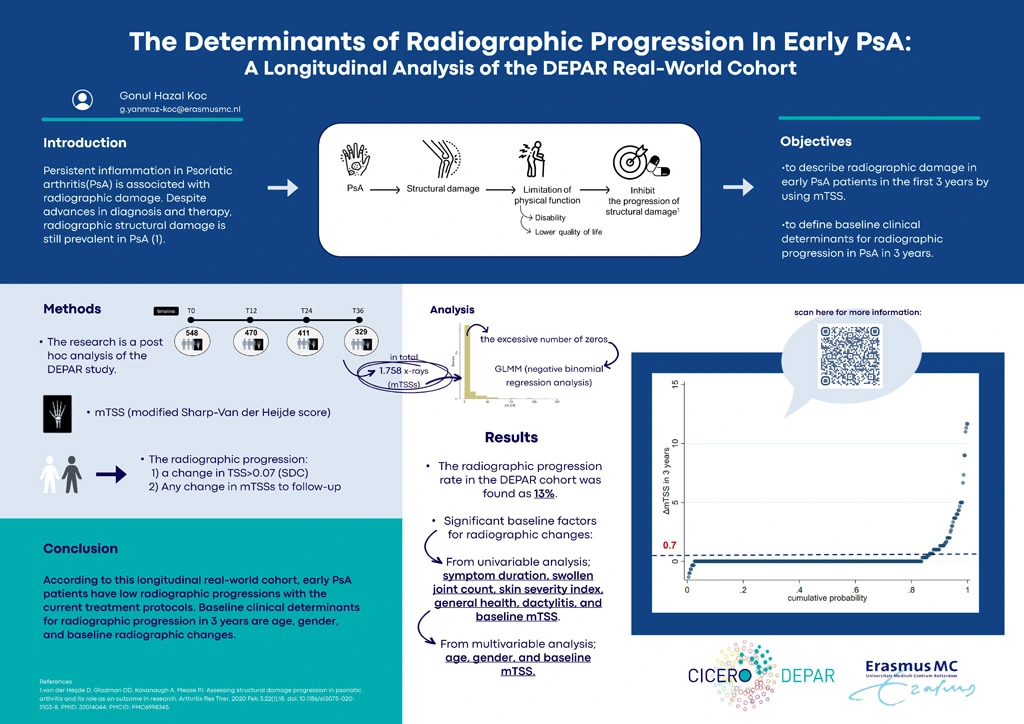
The Determinants of Radiographic Progression In Early PsA: A Longitudinal Analysis of the DEPAR Real-World Cohort
Authors
Keywords
Psoriatic arthritis, Radiography, Outcome Measures, X-ray
Background
Persistent inflammation in Psoriatic arthritis (PsA) is associated with radiographic damage. Despite advances in diagnosis and therapy, radiographic structural damage is still prevalent in PsA (1). To shed light on this topic, we studied which clinical characteristics determine radiographic progression using conventional radiography.
Objective
Our first aim is to describe radiographic damage in early PsA patients. Our second aim is to define baseline clinical parameters as determinants for radiographic progression in early PsA patients in a real-world setting.
Methods
Data from the DEPAR study were used, a cohort comprising PsA patients who were newly diagnosed in real-world data from the modern era. In total 1.758 x-ray pictures were included from 4 different time points (baseline (BL), 1st, 2nd, and 3rd year). Radiographic changes were measured with the modified Total Sharp Score (mTSS) for PsA. The radiographic progression was defined as a change in TSS>0.7 (Smallest Detectable Change) at any time in 3 years of follow-up. Comparisons between groups were made by chi-squared test or ANOVA. Univariable and Multivariable Negative Binomial Generalized Linear Mixed Model (GLMM) analysis was applied to define baseline predictors for radiographic progression over time. Estimates from GLMM were reported by incident rate ratio (IRR).
Results
The study included 1.758 x-ray images of patients from 4 different time points, with median mTSS scores of 0 (0-2), 0(0-3), 0(0-5), and 0(0-6) at T0, T12, T24, and T36 respectively (Table 2). The progressive group (n=63) had a significantly higher mTSS compared to the non-progressive group(n=431) at diagnosis (17(3-36) vs 0(0-1)). A comparison of the two groups revealed that the progressive group had significantly older (59(12) vs 49(13)) and higher swollen joints (93% vs 78%) at diagnosis (Table 3).
In the entire study population, based on the univariable regression analysis, several factors showed significant associations with radiographic outcomes (mTSS) including age, gender, SJC, PASI, VAS, HAQ, Dactylitis, Enthesitis, Baseline mTSS, and biological use during follow-up. After running multivariable analysis, only age, gender, and baseline SHS were found as significant predictors of radiographic changes over time. While old age and high-level baseline mTSSs caused the progression of radiographic outcomes over 3 years, the female gender had a protective effect on radiographic changes (IRR: 0.51, p-value = 0.036) (Table 4).
In only the progressive group, based on univariable regression analysis, this time was found as significant factors are age, symptom duration, SJC, BL CRP, DAPSA, BL mTSS, and biological use in follow-up. After multivariable analysis, there were showed as substantial baseline predictors were only BL DAPSA and mTSS (Table 5).
Conclusions
According to this longitudinal real-world cohort, early PsA patients have low radiographic progressions with the current treatment protocols. Baseline clinical determinants for radiographic progression in 3 years are age, gender, and radiographic changes at baseline (mTSSs>0).
References
- van der Heijde D, Gladman DD, Kavanaugh A, Mease PJ. Assessing structural damage progression in psoriatic arthritis and its role as an outcome in research. Arthritis Res Ther. 2020 Feb 3;22(1):18. doi: 10.1186/s13075-020-2103-8. PMID: 32014044; PMCID: PMC6998345.