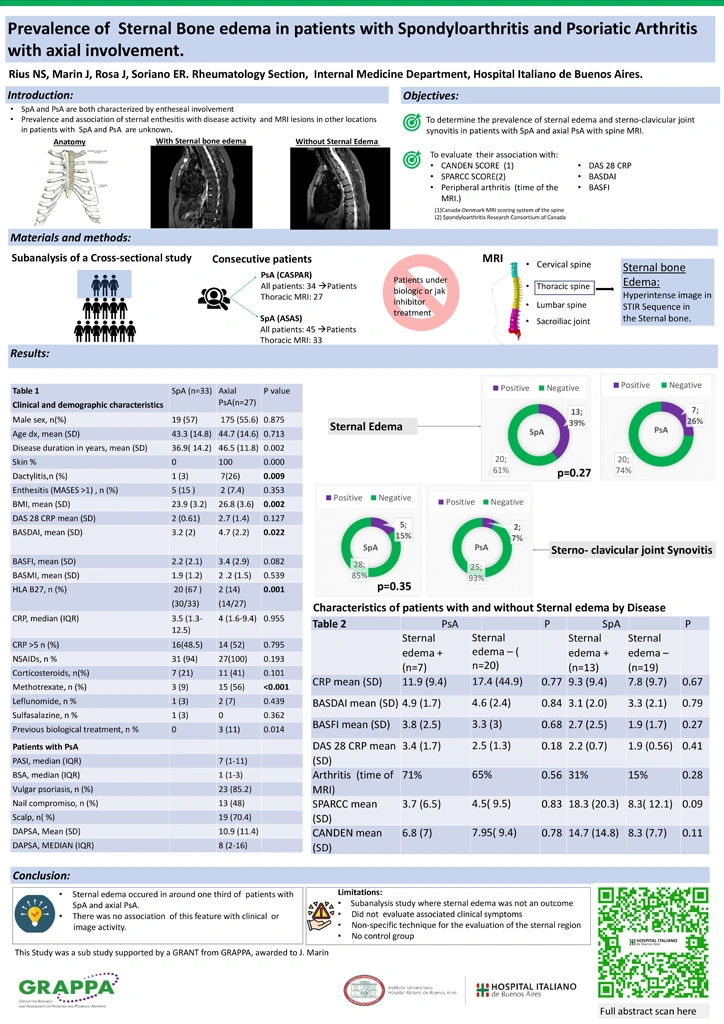
Prevalence of sternal bone edema in patients with spondyloarthritis and psoriatic arthritis with axial involvement.
Introduction:
Spondyloarthritis (SpA) and psoriatic arthritis (PsA) are characterized by entheseal involvement.
Sternal edema is seen as an hyperintense image on magnetic resonance (MRI) STIR sequences in the sternal bone (body or manubrium). For our purposes, we considered sternal edema as a surrogate for enthesitis.
The prevalence and associations of sternal edema with disease activity and other lesions in MRI in patients with SpA and PsA are unknown.
Objective:
The main objective was to determine and compare the prevalence of sternal edema and sterno-clavicular joint synovitis in patients with SpA and axial PsA
We evaluated the association of sternal edema with inflammatory involvement of the spine (CANDEN -Canada Denmark MRI scoring system of the spine) and sacroiliac joints (SPARCC -Spondyloarthritis Research Consortium of Canada Enthesitis Index) score). Also, the association of sternal edema with , DAS 28 CRP, BASDAI, and BASFI scores, and the presence of peripheral arthritis at the time of the MRI as surrogates of clinical activity.
Materials and methods:
We performed a subanalysis of a cross sectional study including consecutive patients with SpA (ASAS criteria) and PsA (CASPAR criteria) with clinical axial involvement. Patients under biologics or jak inhibitor treatment were excluded. Patient´s clinical and demographic characteristics were collected: DAPSA, DAS28CRP, PASI,BSA, MASES score for enthesitis, BASDAI, BASFI, BASMI.
MRI (including STIR sequences) of the sacroiliac joints, cervical, thoracic and lumbar spine were performed, within one month of the clinical evaluation
For sternal bone edema, we evaluated the patients in whom dorsal spine MRI was performed allowing for the visualization of sternum.
The presence of sternoclavicular synovitis was registered.
Results:
Forty five patients with SpA and 34 patients with axial PsA were included but only 33 of SpA and 27 of PsA had dorsal MRI in which sternal edema could be evaluated.
Table 1 shows clinical and demographic characteristics.
Patients with PsA had significantly higher dactylitis, Body Mass Index and disease activity measured by BASDAI.
Thirty nine percent of patients with SpA and twenty six percent of patients with PsA had sternal edema (p 0.271). Sterno-clavicular joint synovitis was found in 15% of SpA patients vs 7.4% of PsA patients (p 0.35).
No association was found between sternal edema and clinical and imaging features. (table 2).
Conclusion:
The prevalence of sternal edema was found in around one third of patients with both SpA and axial PsA. There was no association of this feature with clinical or imaging activity.
Future studies with a larger number of patients might help to define the significance of these findings.