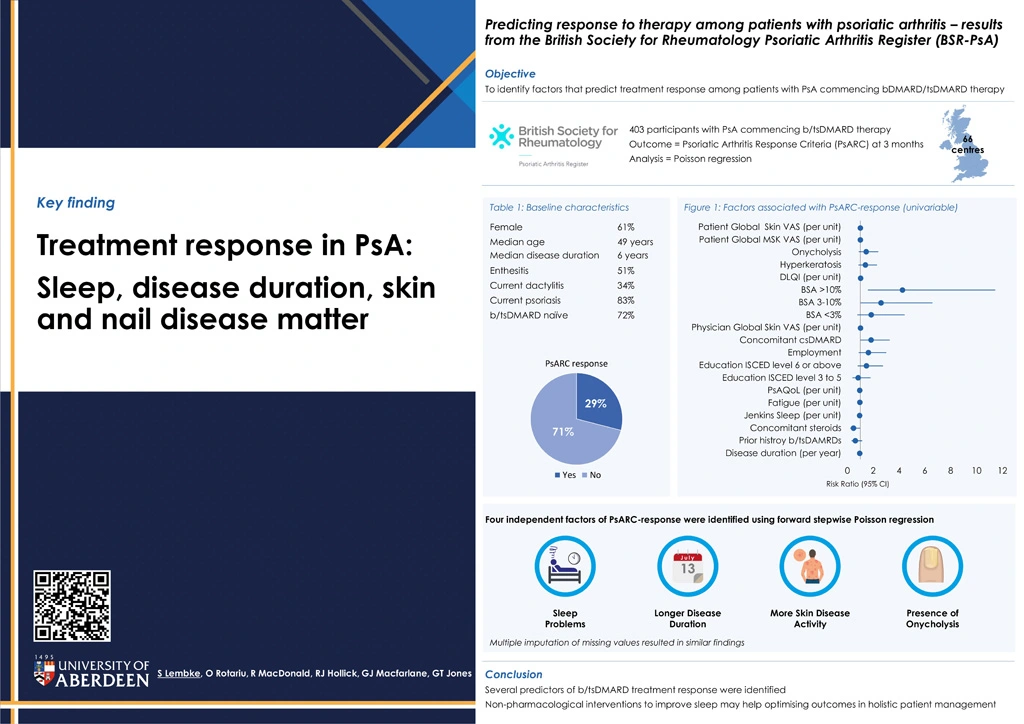
Predicting response to therapy among patients with psoriatic arthritis - results from the British Society of Rheumatology Psoriatic Arthritis Register (BSR-PsA)
Authors
Keywords
Psoriatic Arthritis, Predictors, Treatment Response, Biologic Therapy, Targeted Synthetic Therapy
Background
Given the number of treatment options available in psoriatic arthritis (PsA), identifying predictors of treatment response might inform management plans and help optimise patient outcomes.
Objective
To identify predictors of biologic and targeted synthetic DMARDs (bDMARD/tsDMARD) treatment response.
Methods
The BSR-PsA recruits patients across the UK who satisfy CASPAR-criteria for PsA and are commencing treatment with a bDMARD/tsDMARD they have not previously received, or who are naïve to all bDMARDs/tsDMARDs. Clinical data is collected from medical records, patient-reported outcomes via questionnaires. Predictors of treatment response (PsA Response Criteria (PsARC) at 3 months) were examined using Poisson regression. Univariate predictors of PsARC-response (p≤0.2) were offered to a forward stepwise multivariable model (entry/exit criteria: p≤0.10 and p≥0.15, respectively). A sensitivity analysis was conducted using multiple imputation using chained equations with predictive mean matching to impute missing values.
Results
This analysis used the BSR-PsA January 2023 data download. 403 participants from 66 centres were included (61% female; median age 49yrs; median disease duration 6yrs). 51% had enthesitis, 34% current dactylitis and 83% current psoriasis. 72% were naïve to b/tsDMARD therapy. Most participants were commencing TNF-inhibition (N=285, 71%), and 236 participants (59%) were taking concomitant csDMARDs. PsARC-response was achieved in 45 (29%) patients.
In univariable analysis, factors predicting PsARC-response included a higher level of education, being employed, concomitant csDMARD use, worse skin and nail disease (higher physician global skin assessment, psoriasis body surface area and Dermatology Quality of Life Index; and presence of hyperkeratosis or onycholysis), and poorer patient global musculoskeletal and skin assessments.
In contrast, longer disease duration, prior history of bDMARDs/tsDMARDs, concomitant steroids, poor sleep, high fatigue, and poorer self-reported quality of life were associated with a decreased likelihood of achieving treatment response.
Multivariable complete-case analysis identified the following independent predictors of PsARC-response: poorer sleep (Risk Ratioper 1 unit increase, Jenkins-Sleep-Scale 0.92; 95%CI 0.87-0.96), longer disease duration (RRper year 0.93; 0.87-0.99), physician global skin assessment (RRper 1 unit increase 1.02; 1.00-1.03), onycholysis (RR 1.76; 0.98-3.17). The sensitivity analysis, with imputed data, produced comparable results, suggesting that missing data had not introduced any major bias.
Conclusions
We have identified several predictors of bDMARD/tsDMARD treatment response in PsA that may help improve management. For example, considering non-pharmacological interventions to improve sleep, as part of a holistic management plan, might help to optimise the patient outcomes. Future research might examine whether predictors differ between different agents or modes of action.