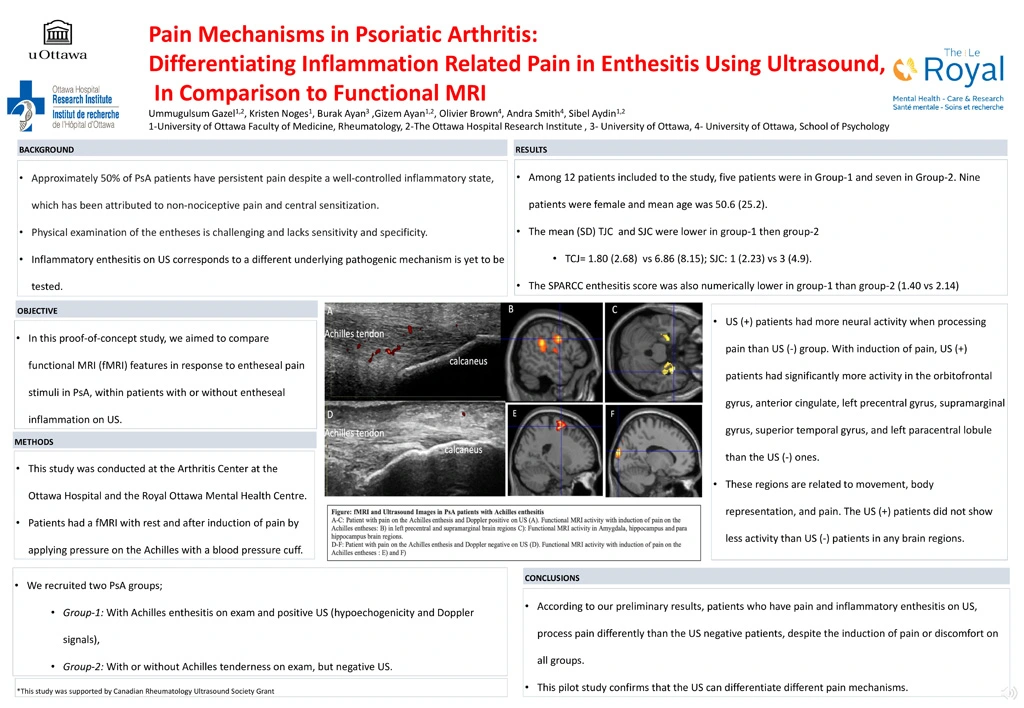
Pain Mechanisms in Psoriatic Arthritis: Differentiating Inflammation Related Pain in Enthesitis Using Ultrasound, In Comparison to Functional MRI
Approximately 50% of PsA patients have persistent pain despite a well‐controlled inflammatory state, which has been attributed to non‐nociceptive pain and central sensitization. Enthesitis is a key domain in PsA. Unfortunately, physical examination of the entheses is challenging and lacks sensitivity and specificity. Ultrasound (US) is used to differentiate inflammatory enthesitis from widespread or non-specific pain syndromes, however whether “inflammatory enthesitis on US” corresponds to a different underlying pathogenic mechanism is yet to be tested.
In this proof-of-concept study, we aimed to compare functional MRI (fMRI) features in response to entheseal pain stimuli in PsA, within patients with or without entheseal inflammation on US.
This study was conducted at the Arthritis Center at The Ottawa Hospital and the Brain Imaging Centre of the Royal Ottawa Mental Health Centre. We recruited two PsA groups; Group-1: With Achilles enthesitis on exam and positive US (hypoechogenicity and Doppler signals), Group-2: With or without Achilles tenderness on exam, but negative US. Patients had a fMRI with rest and after induction of pain by applying pressure on the Achilles with a blood pressure cuff. Whole brain, between group investigations included a two-sample t-test analysis (second level analyses) conducted at a set threshold of p= 0.05 corrected, with a cluster-wise correction at pFWE = 0.05.
Among 12 patients included to the study, five patients were in Group-1 and seven in Group-2. Nine patients were female and mean age was 50.6 (25.2). The mean (SD) TJC and SJC were lower in group-1 (TCJ: 1.80 (2.68), SJC: 1 (2.23)) then group-2 (TJC: 6.86 (8.15); 3 (4.9)). The SPARCC enthesitis score was also numerically lower in group-1 than group-2 (1.40 vs 2.14)
Patients who were US (+) had more neural activity when processing pain than US (-) patients. With induction of pain, US (+) patients had significantly more activity in the orbitofrontal gyrus, anterior cingulate, left precentral gyrus, supramarginal gyrus, superior temporal gyrus, and left paracentral lobule than the US (-) group. These regions are related to movement, body representation, and pain. The US (+) patients did not show less activity than US (-) patients in any brain regions.
According to our preliminary results, patients who have pain and inflammatory enthesitis on US, process pain differently than the US negative patients, despite the induction of pain or discomfort on all groups. This pilot study confirms that the US can differentiate different pain mechanisms.