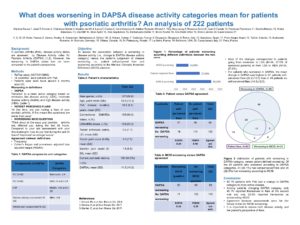
What does worsening in DAPSA disease activity categories mean for patients with psoriatic arthritis? An analysis of 222 patients
Abstract Process
Aenean lacinia dui sed nisl porttitor, sed sodales quam euismod. Fusce et sem quam. Sed in sem quis est hendrerit vestibulum sed at risus. Ut volutpat ornare nulla, vitae ullamcorper sapien imperdiet non. Quisque tristique enim vel purus faucibus fringilla. Ut pellentesque arcu vel rhoncus convallis. Mauris tincidunt elementum dictum. Nunc luctus tortor mattis vestibulum lobortis. Praesent egestas, magna nec viverra feugiat, elit nisl dignissim nulla, non aliquam nisi sem vitae ipsum. In est magna, congue a ipsum sit amet, pulvinar sagittis augue. Nullam et purus egestas, vestibulum dolor eu, dignissim enim. Fusce pretium auctor urna, id volutpat erat tempor vitae. Ut et pharetra arcu, ornare sollicitudin ligula. Pellentesque vel facilisis risus. Mauris vestibulum tortor in quam hendrerit posuere. Ut viverra nibh neque, malesuada gravida orci semper et.
Duis sed purus in lacus pretium commodo. Mauris blandit mattis urna, id malesuada felis efficitur at. Cras tincidunt in urna id aliquet. Nunc ac imperdiet ex. Integer eget dictum enim. Nullam lobortis ut mauris at porttitor. Curabitur iaculis malesuada auctor.

Authors
Marlene Sousa
Josef Smolen
Clémence Gorlier
Maarten Wit
Laura Coates
Umut Kalyoncu
Adeline Ruyssen Witrand
Ying Ying Leung
Rossana Scrivo
Juan Canete
Penélope Palominos
Sandra Meisalu
Andra Balanescu
Uta Kiltz
Sibel Aydin
Inna Gaydukova
Emmanuelle Dernis
Bruno Fautrel
Ana-Maria Orbai
Ennio Lubrano
Laure Gossec
Keywords
outcome measures, PsA, patient perspective
In psoriatic arthritis (PsA), disease activity states are assessed by Disease Activity index
for Psoriatic Arthritis (DAPSA). DAPSA is validated against structural progression. However, the worsening in DAPSA states has not been compared to the patient’s perspective.The objective of this work is to assess the association between a worsening in Disease Activity index for Psoriatic Arthritis (DAPSA) versus the patient’s judgement of disease worsening.
Methods:
ReFlap (NCT03119805) was a longitudinal study in 14 countries with adult patients with PsA for more than 2 years seen twice around 4 months apart (1). Worsening in disease activity between the 2 visits was defined as a transition to a more active category on DAPSA (remission, low disease activity (LDA), moderate disease activity (MDA) and high disease activity (HDA) (2).This change was compared to (a) patient perceived-flare according a patient-reported question: “At this time, are you having a flare of your psoriatic arthritis, if this means the symptoms are worse than usual?”; and (b) a worsening according to the MCID (Minimal Clinical Important Difference) question. The agreement between definitions of worsening were calculated by frequency, Cohen’s kappa and prevalence adjusted bias adjusted kappa (PABAK). No imputation of missing data.
Results:
Overall, 222 patients were analyzed: 127 (58.8%) were male, aged 53.5±12.3 years. On the first visit, disease activity was moderate: 35.9% had no current psoriasis skin lesions, mean tender joint count (TJC, 0-68) was 3.0±7.5, mean swollen joint count (SJC, 0-66) was 1.6±6.6, and mean DAPSA was 11.5±14.0.
At 4.5±2.2 months follow-up, the proportion of DAPSA worsening was 40.1% [95% confidence interval, 33.9-46.7] (n=89). Most of the changes corresponded to patients going from remission to LDA (N=24, 27.0% of worsened patients) or from LDA to MDA (N=24, 27.0%).
Patient-reported flares were reported in 27.0% [21.6-33.2] (n=60), and MCID worsening in 14.0% [33.9-46.5] (n=31).
Of the 89 patients who worsened in DAPSA categories, 41 (46.1%) had self-perceived flares and 20 (22.5%) had worsening by MCID. Among patients who worsened in DAPSA category, the mean change in DAPSA was higher in patients with self-perceived flares (increase of 22.2±15.0) than in patients without self-perceived flares (increase of 14.3±12.3). Of 133 patients with no worsening according to DAPSA, 114 (85.7%) had no self-perceived flares and 122 (91.7%) had no MCID worsening. The kappa [95% confidence interval] (PABAK) coefficients between DAPSA and patient’s flare or MCID worsening were 0.34 [0.21-0.46] (0.40) and 0.16 [0.05-0.27] (0.28), respectively.
Conclusions:
Among patients worsening in DAPSA category, only 46.1% reported themselves in flare at the second visit and 22.5% worsening by MCID. Agreements between DAPSA and patient’s flare and MCID were fair and poor, respectively.