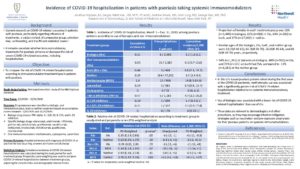
Incidence of COVID-19 hospitalization in patients with psoriasis taking systemic immunomodulators
Abstract Process
Aenean lacinia dui sed nisl porttitor, sed sodales quam euismod. Fusce et sem quam. Sed in sem quis est hendrerit vestibulum sed at risus. Ut volutpat ornare nulla, vitae ullamcorper sapien imperdiet non. Quisque tristique enim vel purus faucibus fringilla. Ut pellentesque arcu vel rhoncus convallis. Mauris tincidunt elementum dictum. Nunc luctus tortor mattis vestibulum lobortis. Praesent egestas, magna nec viverra feugiat, elit nisl dignissim nulla, non aliquam nisi sem vitae ipsum. In est magna, congue a ipsum sit amet, pulvinar sagittis augue. Nullam et purus egestas, vestibulum dolor eu, dignissim enim. Fusce pretium auctor urna, id volutpat erat tempor vitae. Ut et pharetra arcu, ornare sollicitudin ligula. Pellentesque vel facilisis risus. Mauris vestibulum tortor in quam hendrerit posuere. Ut viverra nibh neque, malesuada gravida orci semper et.
Duis sed purus in lacus pretium commodo. Mauris blandit mattis urna, id malesuada felis efficitur at. Cras tincidunt in urna id aliquet. Nunc ac imperdiet ex. Integer eget dictum enim. Nullam lobortis ut mauris at porttitor. Curabitur iaculis malesuada auctor.

Authors
Jonathan Koptyev
Donald and Barbara Zucker School of Medicine at Hofstra/Northwell
Sergey Rekhtman, MD, MPH, PharmD
Donald And Barbara Zucker School Of Medicine At Hofstra/Northwell
Andrew Strunk, MA
Donald And Barbara Zucker School Of Medicine At Hofstra/Northwell
Amit Garg, MD
Donald And Barbara Zucker School Of Medicine At Hofstra/Northwell
George Han, MD, PhD
Donald And Barbara Zucker School Of Medicine At Hofstra/Northwell
Keywords
psoriasis; liver fibrosis; methotrexate; transient elastography
Background:
-
Current research on COVID-19-related outcomes in patients with psoriasis, particularly regarding influence of treatments, is subject to lack of comparator group, selection bias, confounding, and insufficient statistical power.[1]
-
It remains uncertain whether immunomodulatory treatments for psoriasis enhance or decrease the risk of severe COVID-19-related outcomes, including hospitalization.
Objective:
-
To compare the risk of COVID-19-related hospitalization according to immunomodulator treatment type in patients with psoriasis
Methods:
-
Retrospective cohort study of the IBM Explorys database from March 1st, 2020 to December 31st, 2020
-
Drug exposure was classified as biologic, oral immunomodulator, both or neither treatment based on prescription orders between 12/01/2019 and 02/29/2020
-
Biologic drug classes: TNF-alpha, IL-12/IL-23, IL-17A, and IL-23 inhibitors
-
Specific biologic drugs: etanercept, adalimumab, infliximab,
golimumab, certolizumab, ustekinumab, secukinumab,
ixekizumab, brodalumab, tildrakizumab, guselkumab,
risankizumab
-
- Oral immunomodulators: methotrexate, cyclosporine, apremilast
- Primary Outcome: Hospital admission with diagnosis of COVID-19 or positive lab test occurring between admission and discharge
- Statistical Analysis: Cumulative incidence of COVID-19-related hospitalization was calculated during the study period for each treatment group. Propensity score weighting was used to compare COVID-19-related hospitalization between treatment groups, adjusting for comorbidities and demographic characteristics.
Results:
- There were 51,974 psoriasis patients eligible for analysis, of whom 2,593 (5%) received biologics, 1,585 (3%) received OIs, 444 (0.9%) received both, and 47,352 (91.1%) received neither.
- Cumulative incidence of COVID-19-related hospitalization per 1,000 psoriasis patients was 3.1 in the biologics group (8/2,593; 95% CI 1.6-6.1), 9.5 in the OI group (15/1,585; 95% CI 5.7-15.6), 6.8 in those receiving both (3/444; 95% CI 2.3-19.7), and 3.9 in those receiving neither drug class (184/47,352; 95% CI 3.4-4.5).
- Unadjusted RR of COVID-19-related hospitalization for patients taking methotrexate versus neither treatment was 3.73 (95% CI 2.13-6.51), and propensity score-weighted RR was 2.78 (95% CI 1.47-5.26; p=0.002). This translates to an unadjusted risk difference of +11 (95% CI +3, +18) per 1,000 patients and propensity score-weighted risk difference of +9 (95% CI +1, +17) per 1,000 patients.
- Unadjusted RR of COVID-19-related hospitalization for patients treated with biologics compared to those treated with OIs was 0.33 (95% CI 0.14-0.77), and propensity score-weighted RR was 0.35 (95% CI 0.14-0.86; p=0.02). This corresponds to an unadjusted risk difference of -6 (95% CI -12, -1) per 1,000 patients and propensity score-weighted risk difference of -6 (95% CI -11, -0.3) per 1,000 patients, favoring biologics.
Conclusion:
-
In this U.S.-based psoriasis patient cohort during the first wave of the COVID-19 pandemic, methotrexate use was associated with a significantly greater risk of COVID-19-related hospitalization relative to no systemic immunomodulatory treatment.
-
Use of biologics was associated with a lower risk of COVID-19-related hospitalization than use of OIs.
-
These data are relevant to dermatologists and other prescribers, as they may encourage infection mitigation strategies such as vaccination and pre-exposure prophylaxis for their psoriasis patients on systemic immunomodulators.
References:
1. Piaserico S, Gisondi P, Cazzaniga S, Di Leo S, Naldi L. Assessing the Risk and Outcome of COVID-19 in Patients with Psoriasis or Psoriatic Arthritis on Biologic Treatment: A Critical Appraisal of the Quality of the Published Evidence. J Invest Dermatol. 2022;142(2):355-363.e7. doi:10.1016/j.jid.2021.04.036