Early achievement of minimal disease activity in psoriatic arthritis is associated with long-term improvements in quality of life
Abstract Process
Aenean lacinia dui sed nisl porttitor, sed sodales quam euismod. Fusce et sem quam. Sed in sem quis est hendrerit vestibulum sed at risus. Ut volutpat ornare nulla, vitae ullamcorper sapien imperdiet non. Quisque tristique enim vel purus faucibus fringilla. Ut pellentesque arcu vel rhoncus convallis. Mauris tincidunt elementum dictum. Nunc luctus tortor mattis vestibulum lobortis. Praesent egestas, magna nec viverra feugiat, elit nisl dignissim nulla, non aliquam nisi sem vitae ipsum. In est magna, congue a ipsum sit amet, pulvinar sagittis augue. Nullam et purus egestas, vestibulum dolor eu, dignissim enim. Fusce pretium auctor urna, id volutpat erat tempor vitae. Ut et pharetra arcu, ornare sollicitudin ligula. Pellentesque vel facilisis risus. Mauris vestibulum tortor in quam hendrerit posuere. Ut viverra nibh neque, malesuada gravida orci semper et.
Duis sed purus in lacus pretium commodo. Mauris blandit mattis urna, id malesuada felis efficitur at. Cras tincidunt in urna id aliquet. Nunc ac imperdiet ex. Integer eget dictum enim. Nullam lobortis ut mauris at porttitor. Curabitur iaculis malesuada auctor.

Background
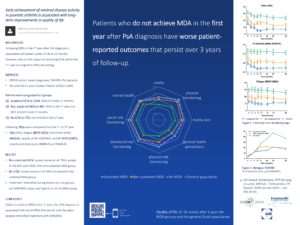
In a previous study we have shown that achieving minimal disease activity (MDA) in the first year after diagnosis is associated with better quality of life (QoL) of psoriatic arthritis (PsA) patients in the first year (1). However, the impact of achieving MDA within the first year on the long-term is lacking.
Objectives
To compare patient-reported outcomes (PROs) from the first to the third year of follow-up between PsA patients who achieved sustained MDA in the first year, patients who achieved MDA in the first year but in whom it was not sustained and patients who did not achieve MDA in the first year after PsA diagnosis.
Methods
Newly diagnosed, DMARD naïve PsA patients with oligo- or polyarthritis and an inclusion date before March 2018, participating in the Dutch southwest Early PsA cohoRt (DEPAR), were selected (2). Patients were categorized in three groups by achievement of MDA in the first year:
- Sustained MDA, includes patients who were in MDA at both their 9- and 12-month visit;
- Non-sustained MDA, includes patients who achieved MDA in the first year but in whom it was not sustained at both 9- and 12-months;
- No MDA, includes patients who did not achieve MDA in the first year.
Background. In a previous study we have shown that achieving minimal disease activity (MDA) in the first year after diagnosis is associated with better quality of life (QoL) of psoriatic arthritis (PsA) patients in the first year (1). However, the impact of achieving MDA within the first year on the long-term is lacking.
Objectives. To compare patient-reported outcomes (PROs) from the first to the third year of follow-up between PsA patients who achieved sustained MDA in the first year, patients who achieved MDA in the first year but in whom it was not sustained and patients who did not achieve MDA in the first year after PsA diagnosis.
Methods. Newly diagnosed, DMARD naïve PsA patients with oligo- or polyarthritis and an inclusion date before March 2018, participating in the Dutch southwest Early PsA cohoRt (DEPAR), were selected (2). Patients were categorized in three groups by achievement of MDA in the first year:
- Sustained MDA, includes patients who were in MDA at both their 9- and 12-month visit;
- Non-sustained MDA, includes patients who achieved MDA in the first year but in whom it was not sustained at both 9- and 12-months;
- No MDA, includes patients who did not achieve MDA in the first year.
The following PROs were measured:
- Pain (VAS)
- Fatigue (BRAF-MDQ)
- Functional ability (HAQ-DI)
- Health-related quality of life (EQ-5D-5L and SF-36 PCS/MCS)
- Anxiety and depression (HADS)
We used a linear mixed model to compare PROs from the first to the third year of follow-up.
Results
Among the 240 patients studied 104 (43%) were classified as sustained MDA, 60 (25%) as non-sustained MDA and 76 (32%) as no MDA. At baseline, patients had a mean (SD) age of 52.8 (14) years and median (IQR) symptom duration of 9.4 (4-31) months. Patients in the no MDA group were more often female and had higher TJC, enthesitis (LEI), HAQ and VAS pain/global scores at diagnosis compared with patients in the sustained MDA group.
In the sustained MDA group, health-related quality of life during follow-up was comparable to the general Dutch population (3). However, patients who did not achieve MDA in the first year scored remarkably poorer on all measured PROs during follow-up, compared with the sustained MDA group. Patients in the non-sustained MDA group also scored significantly worse on PROs, except for SF-36 MCS and HADS, than the sustained MDA group.
Over the years, treatment was intensified in all groups. After 3 years of follow-up, bDMARDs usage was 37%, 19% and 17% in respectively the no MDA, sustained MDA and non-sustained MDA group.
Conclusion
Failure to achieve MDA in the first year after PsA diagnosis is associated with worse patient-reported outcomes that persist over the years despite intensified treatment with bDMARDs.
References:
- Wervers K, Luime JJ, Tchetverikov I, Gerards AH, Kok MR, Appels CWY, et al. Time to minimal disease activity in relation to quality of life, productivity, and radiographic damage 1 year after diagnosis in psoriatic arthritis. Arthritis Res Ther. 2019;21(1):25.
- Kasiem FR, Luime JJ, Vis M, Kok MR, Wervers K, Gerards AH, et al. Lessons learned from clinical phenotypes in early psoriatic arthritis: the real-world Dutch south west Early Psoriatic ARthritis study. Scand J Rheumatol. 2021;50(2):124-31.
- Aaronson NK, Muller M, Cohen PDA, Essink-Bot M-L, Fekkes M, Sanderman R, et al. Translation, Validation, and Norming of the Dutch Language Version of the SF-36 Health Survey in Community and Chronic Disease Populations. Journal of Clinical Epidemiology. 1998;51(11):1055-68.