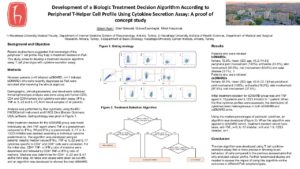
Development of a Biologic Treatment Decision Algorithm According to Peripheral T-Helper Cell Profile Using Cytokine Secretion Assay: A proof of concept
Abstract Process
Each year, GRAPPA invites trainees and junior faculty—assistant professor level, medical/non-medical PhD students, junior post-docs, residents, and fellows—to submit proposals to GRAPPA to fund pilot projects related to psoriasis or psoriatic arthritis. Projects can be in any branch of science: laboratory based, clinical, or epidemiological.

Authors
Keywords
treatment, precision in medicine, T-cell
Background and Objective
Recent studies have suggested that knowledge of the peripheral T cell profile may help in treatment decision in PsA. This study aimed to develop a treatment decision algorithm using T cell phenotype with cytokine-secretion assay.
Methods
Nineteen patients (n=8 initiated csDMARD, n=11 initiated bDMARD) who were recently diagnosed as PsA were recruited after receiving the ethical approval. Demographic, clinical parameters, and blood were collected. Immunophenotype analysis was done using anti-human-CD3, CD4 and CD8 markers and cytokine-secretion assay (IFN-ɣ, TNF-α, IL-22 and IL-17) from blood samples of all patients. Analysis was performed by flow cytometry using the BD-FACSCantoII instrument and FACS Diva (Becton Dickinson, USA) software. Initial treatment decision for the bDMARD group was made individually as; Anti-TNF agent where TNF-α is predominant compared to IFN-ɣ. Where IFN-ɣ is predominant, IL-17 or IL-12/23 inhibitor was decided according to individual cytokine predominance. The algorithm was developed using all patients` results; median values IFN-ɣ, TNF-α, IL-22 and IL-17 cytokines specific to CD4+ and CD8+ cells were calculated. For the initial step, CD4+ TNF- α /IFN ɣ ratio of medians were determined and followed by CD8+ TNF-α /IFN-ɣ ratio of medians. Medians was determined for CD4+ IL-22 and IL-17 as the third step. All ratios and values were taken as cut-offs and an algorithm was developed to choose the best bDMARD (Figure).
Results
Patients who were initiated bDMARDs [female, 72.8%, mean (SD) age, 45.2 (14.5)] had peripheral joint involvement (100%), enthesitis (72.8%), skin involvement (90.9%), nail involvement (63.6%) and axial disease (9.1%). In patients who were initiated csDMARDs [female, 62.5%, mean (SD) age, 45.6 (12.1)] had peripheral joint involvement (100%), enthesitis (18.2%), skin involvement (87.5%), nail involvement (37.5%). Initial treatment decision for bDMARD group was anti-TNF agent in 10 patients and IL12/23 inhibitor in 1 patient. When the final cytokine profiles were assessed, the distribution of cytokines were heterogeneous in both bDMARD and csDMARD arms. Using the median percentages of particular cytokines, an algorithm was developed (Figure). When the algorithm was applied to bDMARD cohort, treatment decision would have been, anti-TNF, n=5; IL-17 inhibitor, n=5 and 1 IL-12/23 inhibitor, n=1.
Conclusion
The new algorithm was developed using T cell cytokine-secretion assay that is more precise in showing the exact behavior of cells compared to the previous assessments that only analyzed cellular profiles. Further randomized studies are needed to assess the impact of using this algorithm on the outcomes in different PsA subphenotypes.