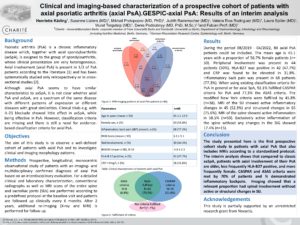
Clinical and imaging-based characterization of a prospective cohort of patients with axial psoriatic arthritis (axial PsA).GESPIC-axial PsA: Results of an interim analysis
Authors
Henriette Käding
Charité-Universitätsmedizin Berlin
Susanne Lüders
Charité - Universitätsmedizin Berlin
Mikhail Protopopov
Charité - Universitätsmedizin Berlin
Judith Rademacher
Charité - Universitätsmedizin Berlin
Valeria Rios Rodriguez
Charité - Universitätsmedizin Berlin
Laura Spiller
Charité - Universitätsmedizin Berlin
Murat Torgutalp
Charité - Universitätsmedizin Berlin
Denis Poddubnyy
Charité - Universitätsmedizin Berlin, Rheumatism Research Centre, Epidemiology Unit
Fabian Proft
Charité - Universitätsmedizin Berlin
Keywords
axial psoriatic arthritis; axial spondyloarthritis
Under the umbrella term spondyloarthritis whose clinical presentations are very heterogeneous, psoriatic arthritis (PsA) and axial spondyloarthritis (axSpA) are subsumed. The presence of axial involvement in patients with PsA (axial PsA) was reported already in 1973 and has been described among others to be present in one third of PsA patients [1]. In the past, retrospective and cross-sectional studies have shown that there are differences in particular: in genetics, clinical presentation, radiographic patterns, as well as in prognostic characteristics [2,3].
This study is a prospective, longitudinal, observational study of axial PsA patients to investigate the clinical and imaging morphology patterns of those patients.
In addition to clinical and laboratory characterization this study is one of the first studies to collect in addition to conventional radiographs, MRI of the whole spine and SIJs according to a standardized protocol from all included patients.
We were able to enroll 88 patients between August 2019 to April 2022. The mean age was 45.1 years with a proportion of 56.8% female patients. HLA-B27 was positive in 42 (47.7%) and C-reactive protein was elevated (>5mg/l) in 28 (31.8%) patients. The modified New York criteria were fulfilled in 45.8% (n=38). The evaluation of the baseline MRIs divided into active and structural changes showed an isolated spinal involvement by 15 patients.
In summary, the baseline data of our cohort showed that axial PsA patients are more likely to be female and less likely to be HLA-B27 positive compared to typical axial SpA patients. Both CASPAR and ASAS criteria were met by 70% of patients. Noteworthy, 17% of the patients showed an isolated spinal involvement without active or structural changes in the SIJs.
References:
- Gladman, D.D., et al., Psoriatic arthritis (PSA)--an analysis of 220 patients. Q J Med, 1987. 62(238): p. 127-41.
- Feld, J., et al., Axial disease in psoriatic arthritis and ankylosing spondylitis: a critical comparison. Nat Rev Rheumatol, 2018. 14(6): p. 363-371.
- Poddubnyy, D., et al., Axial involvement in psoriatic arthritis: An update for rheumatologists. Semin Arthritis Rheum, 2021. 51(4): p. 880-887.