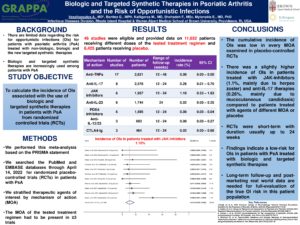
Biologic and Targeted Synthetic Therapies in Psoriatic Arthritis and the Risk of Opportunistic Infections
Biologic and targeted synthetic therapies have changed the management of psoriatic arthritis over the past decades. However, these treatments might result in immunosuppression and could increase risk for opportunistic infections. Here, we present a meta-analysis on the incidence of opportunistic infections among individuals with psoriatic arthritis treated with biologic and targeted agents in randomized placebo-controlled trials. Overall, we found a low-risk for opportunistic infections in patients with PsA treated with biologic and targeted synthetic therapies. Our findings demonstrate a slightly higher incidence of OIs in patients treated with JAK-inhibitors (1.1%, mainly due to herpes zoster) and anti-IL-17 therapies (0.26%, mainly due to mucocutaneous candidiasis) compared to placebo. However, ongoing surveillance, and clinical trials with long-term follow up and post-marketing monitoring are needed to study true opportunistic infections risk in this patient population.
Key References
- Singh JA et al. 2018 American College of Rheumatology/ National Psoriasis Foundation Guideline for the Treatment of Psoriatic Arthritis. Arthritis Rheumatol 2019;71:5-32
- Coates LC et al. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2015 Treatment Recommendations for Psoriatic Arthritis. Arthritis Rheumatol 2016;68:1060-71
- Gossec L et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann Rheum Dis 2020;79:700-12
- Winthrop KL et al. Opportunistic infections and biologic therapies in immune-mediated inflammatory diseases: consensus recommendations for infection reporting during clinical trials and postmarketing surveillance. Ann Rheum Dis. 2015;74(12):2107-16.